Exposure to acute stressors, such as a resolved verbal dispute with your partner or boss, nearly missing a bus or train connection, giving a talk in front of a large audience, applying for a new job, or an intense physical challenge during a sports event are normal everyday situations that tend to make us stronger, not weaker.
In contrast, severely traumatic events (i.e. being raped, a surviving life-threatening car accident, or childhood abuse) as well as long-lasting or chronic external or internal stressors (i.e. chronic disease, an abusive relationship, or being suppressed/exploited in a societal setting) increase the likelihood of developing a stress-related mental disease, such as depression, an anxiety disorder, post-traumatic stress disorder (PTSD), as well as, to a certain degree, addiction and chronic or reoccurring pain. In some of our studies, we therefore work with people that experienced at least 4 traumatic events in their life time, making them an at-risk study population.
The above examples, however, are extremes on a much broader scale. We also know that less severe, but complex transition phases, such as migrating or moving to a new country, moving away from home for the first time to study at a university, enduring a divorce, grieving the loss of a loved one, entering the workforce for the first time, or final exam week at college pose a considerable challenge, and can bring a person to the personal „tipping point” should multiple stressors occur at the same time.
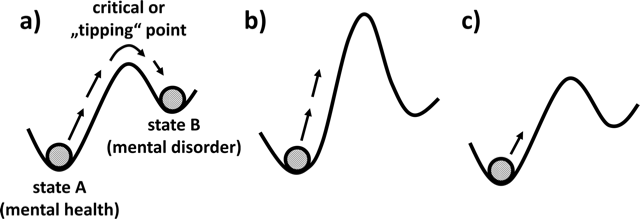
The double-well potential model, applied to psychiatry. a) shows the transition from mental health (state A) to mental disorder (state B). Maintenance of mental health (aka resilience) in the face of adversity (system-activating stressors) may be achieved by b) raising the “tipping point” or c) reducing the overall activation of the system.
The contemporary understanding of stress resilience is the maintenance and/or quick recovery of mental health and overall well-being during and after times of adversity, such as trauma, difficult life circumstances, challenging life transitions, or physical illness.
It is not the same as an indifference towards stressors, or a lack of stress sensitivity. Brain function and synaptic connectivity remains flexible and adaptive throughout life, and it is becoming increasingly clear that resilience – as opposed to lasting stress-induced mental and functional impairments – is the result of a dynamic process of successful adaptation to stressors.
Indeed, there is now ample evidence that individuals change while they successfully cope with stressors, whether this manifests as altered perspectives on life, emerging new strengths or competences, partial “immunisation” against the effects of future stressors, or also as epigenetic alterations and modified gene expression patterns. Hence, resilience is not simply inertia, insensitivity, or a passive response to adversity. In the same vein, resilience can no longer be understood simply as a fixed personality trait. Rather, neurobiological studies indicate that such adaptive, organismic adjustments are causal for the preservation of mental health. This means that we must try to understand the “why and how” behind a positive long-term outcome in the face of adversity if we want to help people maintain mental stability during stressful phases in their life.
Exactly that is the core question of all resilience research. In the DynaMORE project, longitudinal, multidisciplinary studies of people undergoing such stressful transition phases, and mathematical data integration allows us to better understand the dynamic processes behind why and how one individual copes better with the same adversity than a peer in a comparable situation. Once we can successfully apply the gained knowledge to an individual’s personal needs and resilience-enhancing mechanisms via in silico prediction modelling, we may be able to prevent that person from ever reaching the personal „tipping point“.
What we do know is that stress-related mental disorders are multimodal diseases that never just affect one brain region, one organ, or one biomedical process. Rather, all stress-related mental disorders are a complex network of symptoms, some of which are more interdependent than others, driving the person into the disease state. A longitudinal, systems-based approach that allows us to assess a multitude of processes within the body and mind is, thus, the best way of figuring out the temporal and causal interconnectedness of individual symptoms.
Once a key symptom (or symptom network) becomes activated in an individual, we intend to help the person with an established, easily applicable intervention. We will also compare his/her data profile to a gender- and age-matched peer that faces comparable adversity at that time, but does not show activation of this key symptom (or symptom network). What are the stabilising factors for the peer? Can we identify key resilience factors, resilience-enhancing behaviours, and health-maintaining processes?
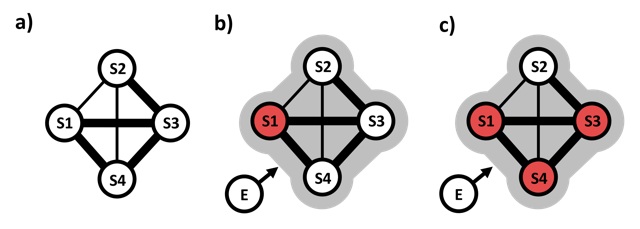
Mental disorders modelled as networks of symptoms. a) shows a symptom (S) network, consisting of nodes S1-S4 that represent symptoms 1-4. No symptom is active, there are no stressors. The system is in a stable state of “mental health”. Strength of positive connections (edges) between symptoms is shown by thickness of lines. S1, S3 and S4 are highly interconnected. In b) an external factor or stressor (E) drives activation of symptom 1 (S1, red). In c), symptoms S3 and S4 are now also active, and the system has reached a new stable state of “mental disorder” characterised by self-sustaining co-activation of the highly interconnected symptoms S1, S3, S4. For simplicity, symptoms are either active (red) or not (white).
Resilience cannot be measured through any one-time assessment, such as a questionnaire, a brain scan, or genotyping before adversity occurs. Instead, we must closely follow the nature and time course of the stressors an individual is exposed to, as well as the changes in mental health that these stressors may or may not induce. Only on this basis can we analyse the adaptive processes that allow individuals to lastingly maintain their mental health despite exposure to stressors and adversity.
Resilience processes may occur at genetic, molecular, physiological, cognitive or behavioural levels, and they include dynamic interactions with the social and non-social environment. Therefore, unravelling the mechanisms that protect the organism from lasting stress-induced dysfunction requires collaboration of biologists, psychologists, clinicians, and social scientists with experts in the mathematical and statistical analysis of complex dynamic systems, especially their modelling and simulation. In this process, laboratory and real-world empirical data about individual reactions to stressors as well as existing knowledge about causal relationships between different factors need to be integrated and translated into formal models.
The models then need to be validated in empirical studies. Such empirical studies must not only be observational but must also involve interventional approaches, where identified resilience factors are manipulated experimentally in real life, in order to verify their causal role. Empirical model testing, in turn, can be used to refine a model and so forth. Such an approach can generate new mechanistic insights that cannot be gained from purely empirical studies or non-formal theorising.
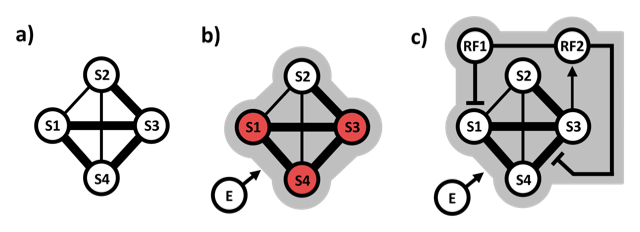
Resilience model: simplified hybrid network incorporating resilience factors. A network with highly interconnected symptom nodes S1, S3, S4 (a) is easily driven into synchronised symptom activation by an external stressor (E) (red nodes in b). In c) this is avoided because resilience factor 1 (RF1) inhibits activation of symptom S1 and resilience factor RF2 inhibits spread of activation between symptoms S3 and S4. In the example, RF1 and RF2 promote each other (they are connected), and RF2 is activated by symptom S3. E may also drive RF activation.

